How bacteria in the mouth may offer new clues to cognitive dysfunction in people with schizophrenia
Study shows associations between oral microbiota diversity and cognitive function
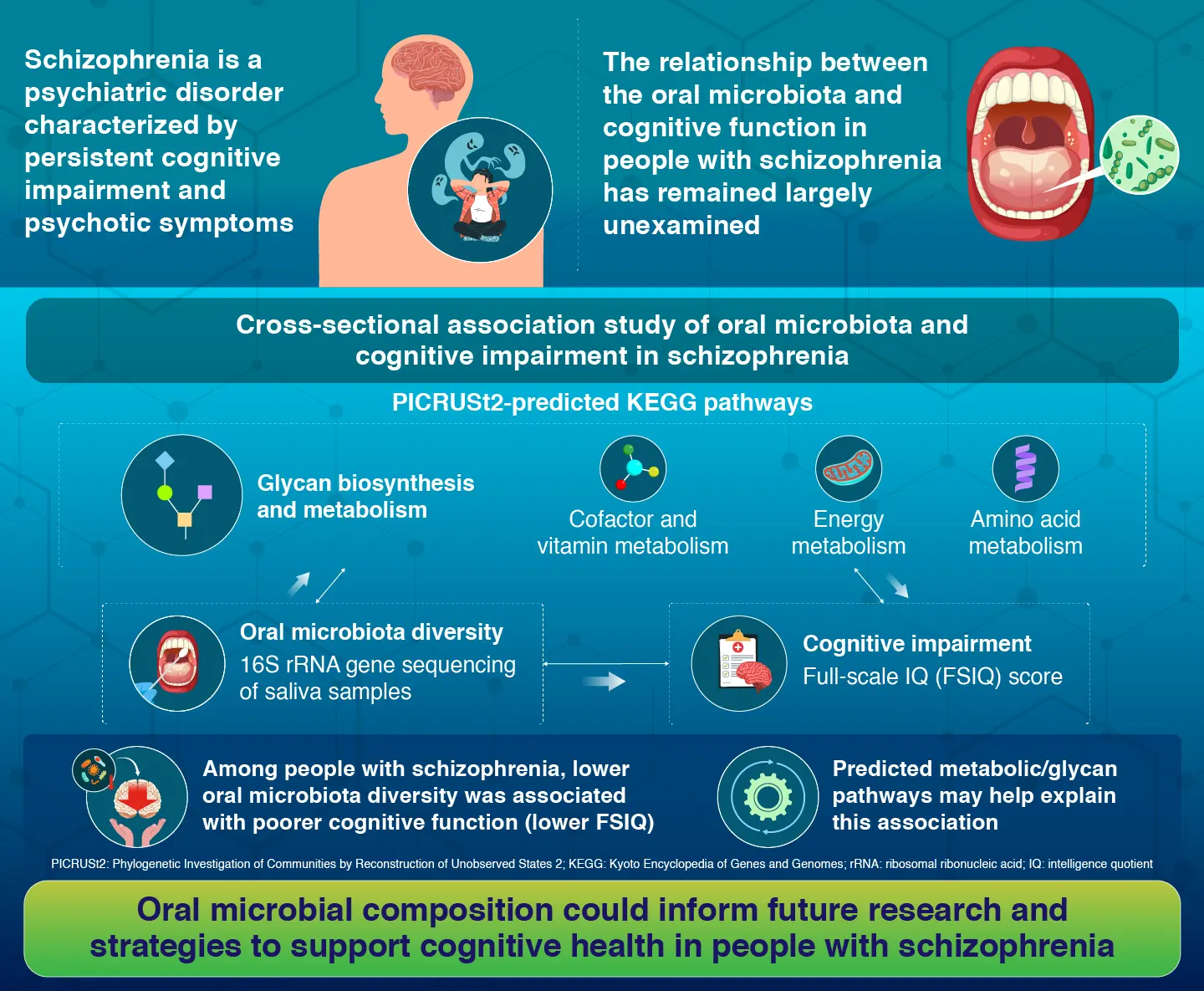
An association between oral microbiota and cognitive performance in schizophrenia has been reported by researchers at Science Tokyo. By analyzing saliva samples and cognitive test scores from patients with schizophrenia and healthy controls, the study shows that lower oral microbial diversity is associated with poorer cognitive function, with specific predicted microbial metabolic pathways potentially linked to this relationship. These association patterns offer testable hypotheses for future longitudinal and experimental studies.
Microbes in the Mouth May Hold Clues to Cognitive Impairment in People with Schizophrenia
Schizophrenia is a debilitating mental illness characterized not only by hallucinations and delusions, but also by persistent cognitive deficits that can severely limit a person’s ability to work, socialize, and live independently. While scientists have long suspected that microbes in the body may contribute to this cognitive decline, research has traditionally focused on the gut. Increasing evidence now suggests that the community of bacteria living in the mouth may also play an important role.
A recent study by researchers at Institute of Science Tokyo (Science Tokyo), Japan, shifts attention to the "oral–brain axis," examining whether changes in the oral microbiota are associated with cognitive impairment in schizophrenia and exploring how this relationship might arise.
The study, published online in the journal Schizophrenia Bulletin on November 27, 2025, was led by Assistant Professor Takehiro Tamura, Associate Professor Genichi Sugihara, and Professor Hidehiko Takahashi of the Department of Psychiatry and Behavioral Sciences, Graduate School of Medical and Dental Sciences, Science Tokyo, together with Assistant Professor Yujin Ohsugi and Professor Sayaka Katagiri of the Department of Oral Biology, Graduate School of Medical and Dental Sciences/Section of Oral-Systemic Health, Oral Science Center, Institute of Biomedical Engineering, Science Tokyo.
"Host–microbiome interactions are not limited to the gut. Like the gut microbiota, the oral microbiota also participates in such interactions. Its significance in systemic and neurological conditions has become increasingly recognized," says Tamura.
The researchers hypothesized that disruptions in the oral bacterial ecosystem could be linked to poorer cognitive performance, either through increased inflammation or through changes in essential microbial functions. To investigate this, they compared 68 patients with schizophrenia and 32 healthy individuals.
Cognitive ability was assessed using the Wechsler Adult Intelligence Scale-Fourth Edition and the Japanese Adult Reading Test, with overall cognitive performance summarized by the full-scale intelligence quotient (FSIQ), where higher scores indicate better cognitive function. To characterize the oral microbiota, saliva samples were collected and analyzed using 16S rRNA gene sequencing. The researchers then used a computational tool called Phylogenetic Investigation of Communities by Reconstruction of Unobserved States 2 (PICRUSt2) to predict the functional potential of the microbial communities based on their genetic profiles.
To evaluate inflammation that could affect brain function, the study measured activity in the kynurenine pathway, a metabolic pathway linked to immune activation and often used as an indirect indicator of neuroinflammation.
The results showed a clear association between oral microbiota diversity and cognitive performance. Patients with schizophrenia had less diverse oral bacterial communities and performed worse on cognitive tests. Within the schizophrenia group, lower microbial diversity was associated with lower FSIQ. The oral microbiota of patients also showed an imbalance in key bacterial groups, with a higher ratio of Streptococcus to Prevotella, along with changes in other prominent genera.
Further analyses suggested that PICRUSt2-predicted microbial functional pathways related to glycan biosynthesis, energy metabolism, and cofactor production were positively associated with cognitive performance. These pathways may provide functional clues to how oral microbiota diversity relates to cognition. In contrast, markers of the kynurenine pathway did not show evidence of a mediating role in this association. As a cross-sectional study with computationally predicted functional profiles, the findings are hypothesis-generating.
"In people with schizophrenia, lower oral microbiota diversity was associated with poorer cognitive performance, and certain metabolism- and glycan-related functional pathways (PICRUSt2-predicted) were suggested to be potentially involved in this relationship," explains Tamura.
The findings suggest that alterations in the oral microbiota are associated with cognitive dysfunction in people with schizophrenia, highlighting the oral microbiome as an accessible window into microbial states linked to cognition. These results open new directions for understanding cognitive impairment and for testing oral care and microbiome-targeted approaches.
"This study offers a new perspective on the oral–brain axis and lays a foundation for future mechanistic studies and intervention research, the latter including studies of oral hygiene measures, prebiotics, and probiotics," adds Tamura.
Reference
- Authors:
- Takehiro Tamura1*, Yujin Ohsugi2,3,4, Sayaka Katagiri2,3, Ayako Kusano1,5, Takehisa Handa1,6, Peiya Lin2,3, Anhao Liu7, Keita Toyoshima8, Shunsuke Takagi1, Hiroki Shiwaku1, Genichi Sugihara1, and Hidehiko Takahashi1,9
*Corresponding author - Title:
- Oral Microbiota Associated With Cognitive Impairment in Schizophrenia: Composition and PICRUSt2-Predicted Functional Pathways
- Journal:
- Schizophrenia Bulletin
- Affiliations:
- 1Department of Psychiatry and Behavioral Sciences, Graduate School of Medical and Dental Sciences, Institute of Science Tokyo, Japan
2Department of Oral Biology, Graduate School of Medical and Dental Sciences, Institute of Science Tokyo, Japan
3Section of Oral-Systemic Health, Oral Science Center, Institute of Biomedical Engineering, Institute of Science Tokyo, Japan
4Section of Vascular Cell Biology, Joslin Diabetes Center, Harvard Medical School, United States
5Department of Child and Adolescent Psychiatry, Tokyo Metropolitan Otsuka Hospital, Japan
6Department of Physiology and Cell Biology, Graduate School of Medical and Dental Sciences, Institute of Science Tokyo, Japan
7Department of Periodontology, Graduate School of Medical and Dental Sciences Institute of Science Tokyo, Japan
8Department of General Dentistry, Graduate School of Medical and Dental Sciences Institute of Science Tokyo, Japan
9Center for Brain Integration Research, Institute of Biomedical Engineering, Institute of Science Tokyo, Japan
Related articles
Further information
Assistant Professor Takehiro Tamura
Department of Psychiatry and Behavioral Sciences, Graduate School of Medical and Dental Sciences, Science Tokyo
Contact
Public Relations Division, Institute of Science Tokyo
- Tel
- +81-3-5734-2975
- media@adm.isct.ac.jp