Pioneering next-generation medicine with placental organoids—Hirokazu Kaji
Unlock your curiosity: Step into the world of science!

Professor Hirokazu Kaji has successfully fabricated a placental organoid to replicate the barrier function of the placenta, one of the least-researched internal organs. His sheet-shaped placental barrier model allows us to estimate what substances, and in what quantities, can pass through the placenta and impact the fetus. This model is expected to replace animal experiments, which are not fully applicable to humans, in the development of drugs, supplements, and foods that minimize side effects on the fetus.
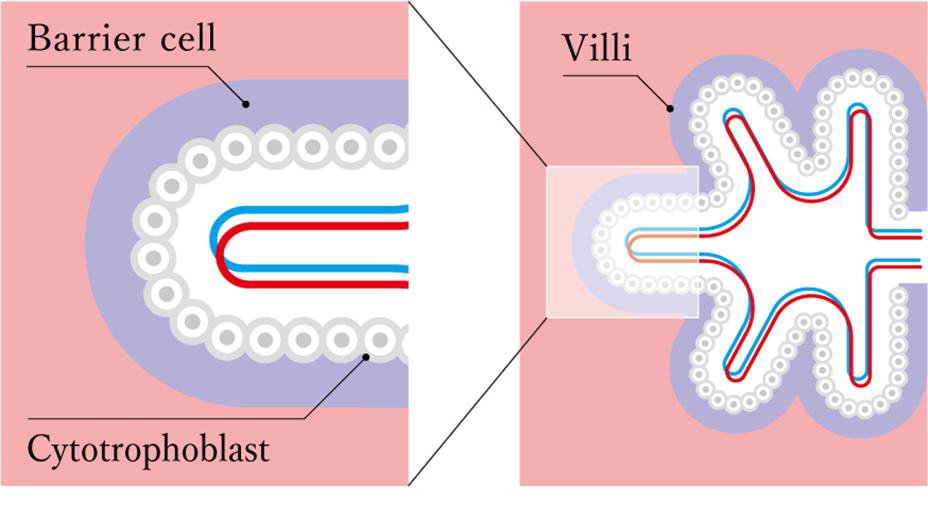
The placenta is essential for fetal development. It is an important organ with various functions. Among these, researchers and stakeholders in the medical and drug discovery fields are particularly focused on its barrier function, which protects the fetus from hazardous substances and viruses from the outside. The numerous villi found in the placenta act as filters, guarding the fetus against harmful substances. However, these villi are not infallible; substances like nicotine and caffeine can still be transported to the fetus because their molecular mass is small enough to pass through. This is why pregnant women are advised to refrain from consuming them. Additionally, certain medications and viruses can also pass through the placenta, negatively impacting the fetus. Therefore, in drug development, it is crucial to accurately determine the placental permeability of target substances and the amounts transported to the fetus.
However, many mysteries surround the placenta, often described as the least studied organ. A significant portion of the mechanisms behind placental permeability remains unknown. This research lag can be attributed to the difficulty of extrapolating data from animal experiments to humans due to the substantial differences in placental structure among animal species. There has been a report of a case where a pregnant woman took a medication that did not show any anomalies during animal studies, yet it led to congenital malformations in the child. Additionally, obtaining healthy, undamaged human placentas is challenging, making it difficult to conduct accurate experiments and leading to the delay in research.
Professor Hirokazu Kaji of the Laboratory for Biomaterials and Bioengineering has illuminated the path to unraveling the mechanisms of placental permeability. An expert in medical engineering, Kaji has successfully produced placental organoids from human trophoblast stem (TS) cells nurtured at Tohoku University School of Medicine, effectively reproducing a sheet-shaped placental barrier model. This development enables the quantitative estimation of the placental permeability of target substances, which is expected to be useful for enhancing medical procedures and developing drugs that minimize side effects on the fetus. Safety testing using this model — which replaces traditional animal experiments — is likely to address ethical issues and accelerate drug development. Additionally, the model is anticipated to be valuable for research in various areas, such as the mechanisms of placental formation and pregnancy-related diseases. We interviewed Professor Kaji about this innovative technology, which sheds light on the future of placental research.
Pick up
Placenta supports the growth of the fetus
The placenta is an organ that serves as a liaison between the mother's body and the fetus. It plays a vital role in the fetus's growth by supplying nutrients and oxygen through its blood vessels and transporting waste products from the fetus.
Barrier function to block hazardous substances
When substances are sent from the mother's body to the fetus, those that have adverse effects on the fetus are filtered out. This filtering is made possible by barrier cells known as "syncytiotrophoblasts," which act as filters. These barrier cells, along with cytotrophoblasts cover the villi, which are densely found within the placenta.
Umbilical cord connects the placenta to the fetus
The umbilical cord is a string-like structure that transports blood from the placenta to the fetus and carries waste products from the fetus back to the placenta.
"The placental barrier model will be key to unlocking the mysteries surrounding the placenta, an organ into which research significantly lags behind"

Repeated trials and errors in reproducing the barrier function lead to a practical model after persistent research
Organoids are three-dimensional tissues produced from cultured Stem cells[1] in vitro, which replicate the functions of an organ. They are valuable in fields such as medicine, biology, and pharmacy because they enable us to understand complex organ structures. Historically, no human trophoblast stem (TS) cells were available, which forced researchers to rely on models made from cancerous villi cells. Since such cells are not healthy tissues, this compromised the accuracy of the data obtained. While conducting research using this inadequate model, I learned that a research team at Tohoku University School of Medicine, with whom I have long collaborated, had succeeded in developing technology to nurture human TS cells. One of the researchers with whom I worked reached out to ask about the utility of these stem cells in research. This prompted me to begin developing a human placental organoid that replicates the villi structure, aiming to unlock the mysteries surrounding the placental barrier function, which directly impacts the health of both the mother and the fetus.
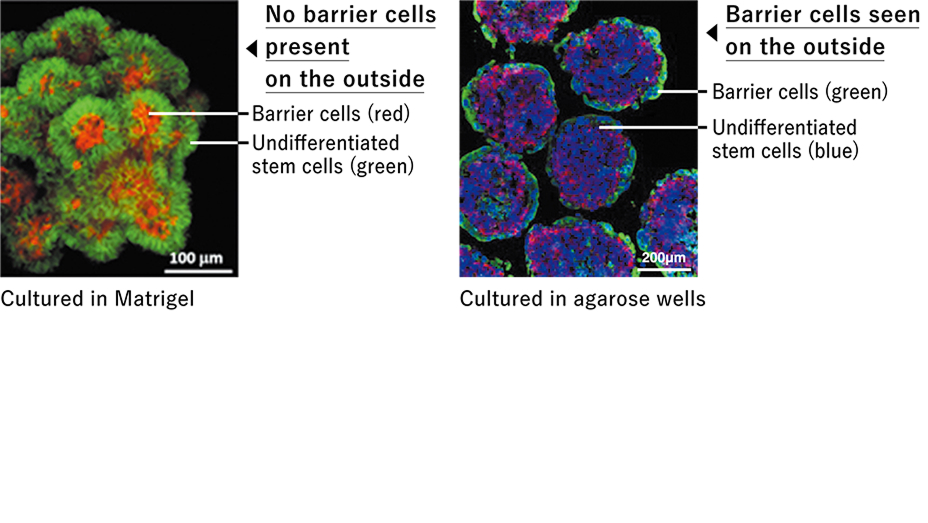
Research is never easy and typically involves many twists and turns. I used Matrigel, a cell scaffold commonly utilized for creating organoids. The resulting organoid featured barrier cells on the inside and undifferentiated placental stem cells on the outside, which is the reverse of the actual villi structure. As I went through trials and errors to invert the structure, I discovered that agarose microwells (plates with fine indentations) are effective as scaffolds. Using this scaffold, we cultured placental stem cells for eight days, and finally succeeded in creating spherical organoids with the barrier cells on the outside and undifferentiated stem cells on the inside. We observed that the cells on the surface of the completed organoid integrated seamlessly, much like the actual villi.
Completing an organoid is not the ultimate goal; rather, our objective is to measure the placenta's permeability to substances. A spherical organoid has a limitation in that it does not allow for an accurate evaluation of permeability. Its spherical shape is unsuitable for quantitatively assessing the amounts of substances passing through the villi. To address this issue, we began developing a sheet-shaped placental barrier model by applying the formation conditions of placental organoids.
We discovered that culturing stem cells on a collagen membrane results in flat organoids, successfully reproducing the double-layer structure of barrier cells and undifferentiated placental stem cells across a wide area of the sheet.
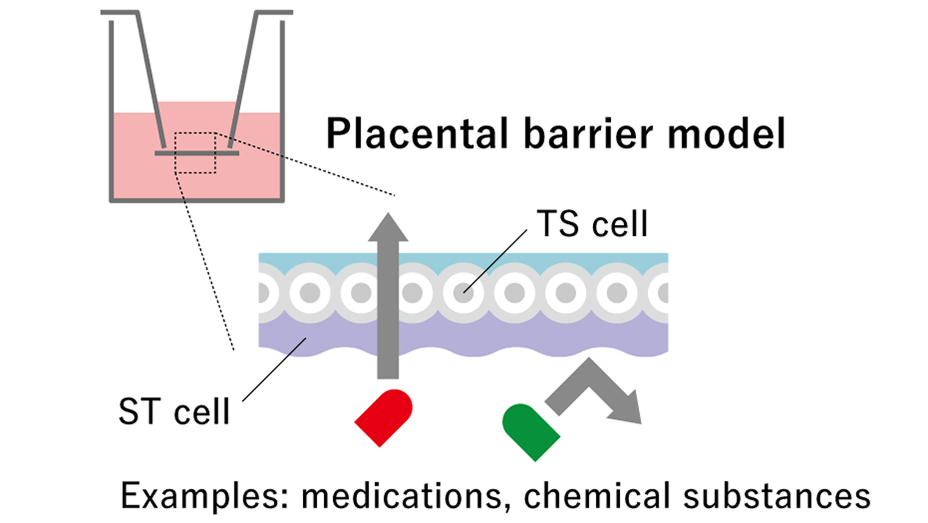
This model is easy to use. We can investigate how much substance permeates by placing a liquid solution under the sheet and measuring the amounts of solutes that pass through to the upper part of the sheet. Verification with the sheet indicated that it exhibits traits similar to those of the actual placenta concerning substances known to have permeability.
We have received inquiries about the model from various sources, and it has now proven to be useful for research. In particular, the model is expected to be used in drug discovery and food development to evaluate the safety of new drugs and food products. The model can be used instead of animal experiments to assess the safety of drugs and supplements, offering data like that derived from human placentas and shortening the verification time. In the future, I aim to establish a framework to certify maternity supplements that have undergone safety evaluations using this model.
How to evaluate the permeability of substances using the sheet-shaped placental barrier model
In the double-layer structure, barrier cells (ST cells) in the lower layer act as filters, blocking or allowing medicines or pathogens to pass through. Substances that are blocked will move to the sheet's lower section, while substances that are allowed to pass will be transported to the upper section.
Organoids cultured on Matrigel or agarose
On the left is a photo of an organoid cultured in Matrigel. The barrier cells, which should be on the outside, are positioned inside, revealing an inside-out structure, in contrast to the correct configuration. On the right is a photo of an organoid cultured in agarose, cut in half. Similar to normal placental villi, the barrier cells are assembled on the outside.
"Designing research by following my curiosity about topics I find intriguing, and by engaging in free thinking. Always aiming at advancing medical care and research"
A future of medical care and research contributed by biomaterials-materials of biological origin
My laboratory is advancing medical engineering research based on micro- and nano-technologies using biomaterials (materials of biological origin). Our research topics include biomimetic systems Biomimetics systems[2] , such as placental organoids, implantable medical devices, and cell delivery systems. For example, we are developing a drug delivery system for patients with diseases in the posterior segment of the eye. A small device containing the drug can be affixed to the area behind the eye, which eye drops cannot reach, to continuously administer a small amount of the drug, thereby alleviating the patient's burden.
Research related to living bodies, such as transplant medicine and biopharmaceuticals, is advancing today. There are medical fields where conventional products are ineffective, so our research aims to assist those areas by developing new biomaterial technologies.
The potential for collaboration is limitless. Innovative ideas lead to technologies that benefit people
I encountered the field of medical engineering while studying at the Massachusetts Institute of Technology (MIT) as part of my doctoral program at a Japanese university. My area of specialization was originally physical chemistry. At MIT, I studied under Professor Robert Langer, a pioneer in the in vitro fabrication of tissues and internal organs, which drew me to biomaterial research, a field that was attracting significant attention at the time. Robert, whom I consider a genius, attracted many unique researchers around him, greatly inspiring me. This experience made me realize that there are people who can come up with such unique ideas and how vast this world truly is.
The broad perspectives I acquired as a young researcher continue to influence my flexible approach today. I aim to cultivate collaborative relationships with researchers from as many diverse fields as possible and contribute with my technology. I have no hesitation in pursuing paths that intrigue me. My proactive nature helps me foster connections with researchers in other domains, broadening the scope of collaboration. I often approach other fields as somewhat of a novice, offering ideas that experts might not conceive. I have high hopes that the merger of Tokyo Institute of Technology and Tokyo Medical and Dental University will accelerate collaboration between medicine and engineering. I am committed to continuing my research to contribute to advances in research and medical treatments through medical engineering technology, ultimately benefiting as many patients as possible.
Glossary
- [1]
- Stem cells: Stem cells are involved in cell regeneration and production. They are able to replicate themselves (production of cells with the same properties), and they can differentiate into various cell types within the body. Stem cells derived from the placenta are called placental stem cells (TS cells), and they are capable of self-replication and differentiation into the cells that constitute the placenta.
- [2]
- Biomimetics systems: Biomimetic systems involve cells from living organisms artificially cultured in vitro in three dimensions, such as organoids, which replicate the functions of an organ, and organs-on-chips. They are used in various applications, including evaluating drug effectiveness and side effects, as well as studying the mechanisms of diseases and biological functions.
My future research
Enhancing our presence in the placental research field by providing the world’s first placental barrier model
Kaji: In 2023, we launched a joint venture firm, HPS Inc., with the aim of promoting the use of the placental barrier model we developed. We plan to provide this model to companies and research institutes for evaluating the placental permeability of medications and functional foods. Our placental barrier model, which is designed to quantitatively evaluate substances, is the first of its kind in the world. In the future people may say that Japan is the leader when it comes to assessing placental permeability. However, the significance of biological devices, not limited to this model, is fully realized only when they are actively used. I aim to convey the benefits of these devices and promote their technologies.。
Profile
Hirokazu Kaji
Professor Hirokazu Kaji, Laboratory for Biomaterials and Bioengineering, Institute of Integrated Research

In 2005, Professor Kaji completed a doctoral program in bioengineering and robotics at the Graduate School of Engineering, Tohoku University. After becoming an overseas research fellow of the Japan Society for the Promotion of Science in 2009, he assumed the position of associate professor at Tohoku University's Graduate School of Engineering in 2011. In 2021, he moved to Tokyo Medical and Dental University (now Science Tokyo), where he is a professor in the Laboratory for Biomaterials and Bioengineering. Additionally, he serves as the chief technology officer and a board member at HPS Inc.
Related articles
Interview held on November 21, 2024
Update history
- The title of this article was updated on Oct 21, 2025